Part 2 of 5: Mental Health Changes after the Onset of COVID-19
The impact of COVID-19 has led to widespread concerns about its unique effects on college student’s mental health. To examine this topic more broadly, CCMH is completing a five-part blog series using a wide range of longitudinal clinical data from students seeking mental health services at college counseling centers nationally.
In Part 1 of 5, CCMH explored the relationship between COVID-19, reasons for seeking treatment, and mental health impacts. Expanding on these findings, Part 2 of 5 will zoom out to compare students who sought treatment before COVID-19 to those who sought treatment after the onset of COVID-19. Data from Fall 2019 were compared to data from Fall 2020, including clinical information from students and clinicians gathered via the Counseling Center Assessment of Psychological Symptoms (CCAPS) and the Clinician Index of Client Concerns (CLICC) at students’ initial appointments. This blog will explore the following questions:
- Did students’ self-reported psychological distress change from Fall 2019 to Fall 2020?
- Did students’ presenting problems, as assessed by clinicians, change from Fall 2019 to Fall 2020?
Did students' self-reported psychological distress change from Fall 2019 to Fall 2020?
Counseling center members of CCMH ask each student to complete the CCAPS to measure various domains of psychological distress at their first appointment (sometimes called an intake). Using data from 82,241 students seeking services from 74 counseling centers, CCMH examined changes in average psychological distress from Fall 2019 (7/1/2019 – 11/30/2019) to Fall 2020 (7/1/2020 – 11/30/2020). The charts below illustrate these data by plotting the average raw scores for each CCAPS subscale over time (i.e., the average daily level of distress at intake) by year, with Fall 2019 in red and Fall 2020 in blue. Overlapping lines indicate no differences between the two years.
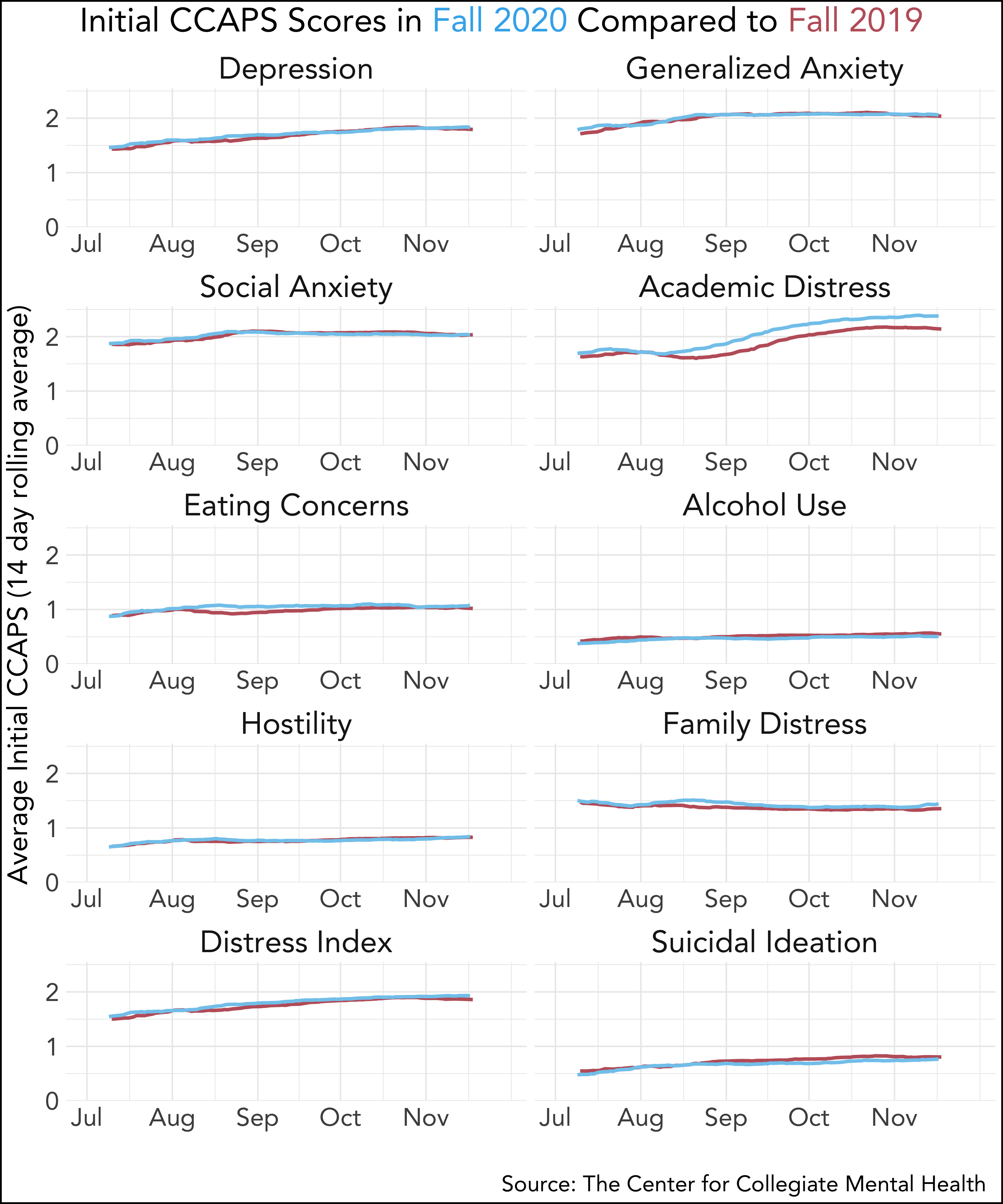
In general, students’ self-reported average distress during Fall 2020 looks quite similar to their average distress during Fall 2019, with some notable variations. Eating Concerns and Family Distress demonstrated slight and temporary increases from mid-August to mid-September 2020. Specific symptoms of the Eating Concerns subscale that contributed to its increase were: thinking about food more than they would like, feeling better when they eat less, and dissatisfaction with their weight. Family Distress increased primarily due to students reporting that their family is getting on their nerves, experiencing unhappiness in their family, feeling unloved by their family, and reporting a history of abuse in the family. While these increases appear to be slight and temporary, they are significant and consistent with clinician experiences.
Academic Distress demonstrated a larger and more sustained increase from 2019 to 2020. The items that drove this increase included experiences such as a lack of motivation for classes, trouble concentrating, inability to complete work, and lack of enjoyment of classes. In comparison to the temporary elevations observed in Eating Concerns and Family Concerns, Academic Distress was substantially more elevated and constant over time, suggesting that students were reporting these impacts regardless of when they sought services during the semester.
Other domains of distress measured by the CCAPS (Depression, Generalized Anxiety, Social Anxiety, Alcohol Use, Hostility, General Distress, and Suicidal Ideation) were relatively stable between 2019 and 2020. There were several noteworthy findings when CCMH delved deeper into the specific symptoms of Depression and Generalized Anxiety. First, feelings of isolation and being alone, a symptom on the Depression subscale, increased considerably from 2019 to 2020. Second, several symptoms of Generalized Anxiety, including sleep difficulties, being easily frightened, racing thoughts, general fear, and tension increased from 2019 to 2020. These increases were offset by another symptom of Generalized Anxiety (anxiety about having a panic attack in public) that significantly decreased. This suggests that specific aspects of depression and anxiety (that are broadly consistent with social isolation and fear/uncertainty) increased after the onset of COVID-19, whereas other symptoms did not.
Did students’ presenting problems, as assessed by clinicians, change from Fall 2019 to Fall 2020?
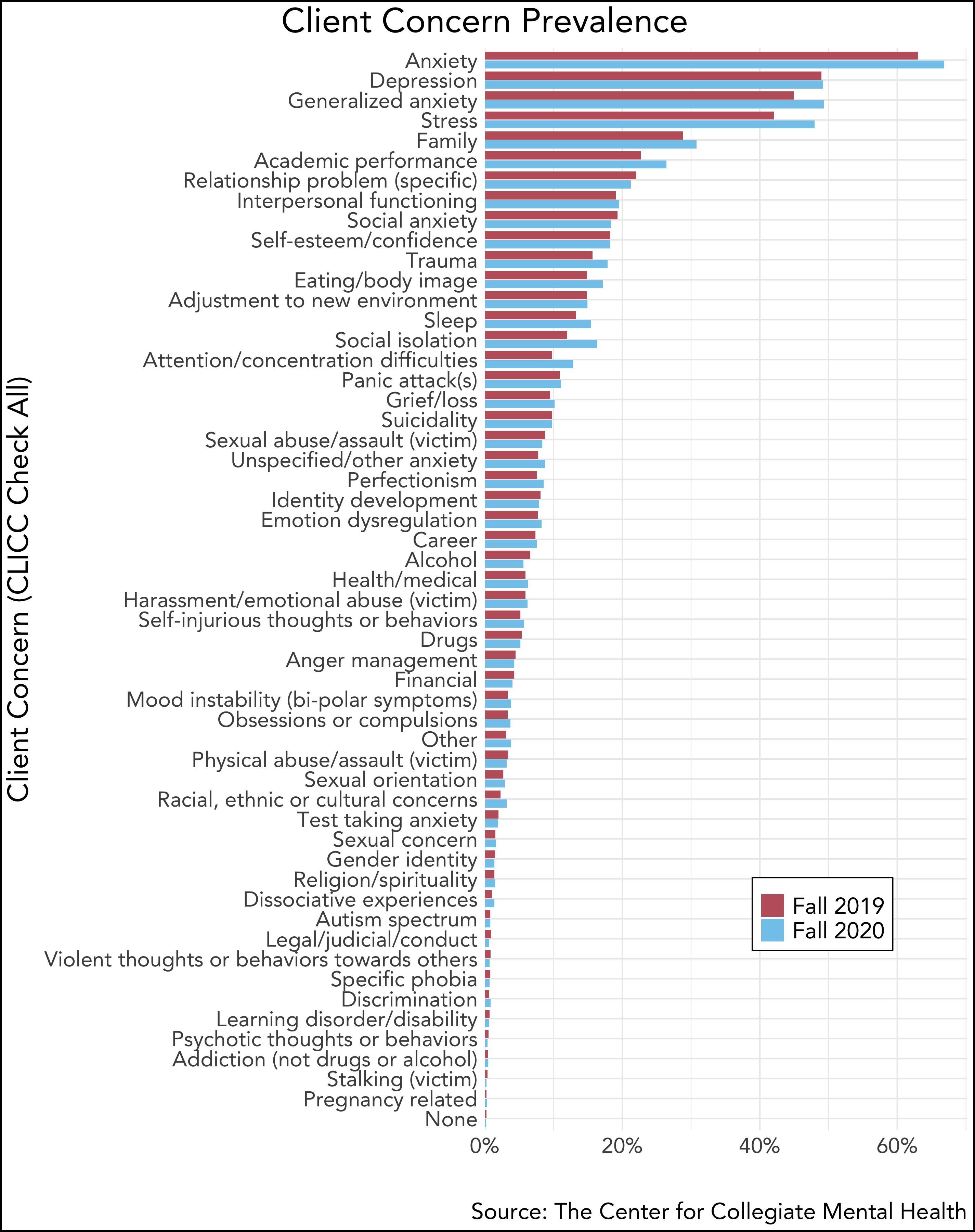
Counseling center members of CCMH also ask clinicians to provide standardized clinical data on students after the initial appointment using the CLICC. Utilizing data from 41,802 students seeking services at 44 counseling centers, CCMH evaluated the degree to which student presenting concerns changed from the Fall 2019 (7/1/2019 – 11/30/2019) to 2020 (7/1/2020 – 11/30/2020).
The table below illustrates how often each presenting concern was identified by clinicians (prevalence) during Fall 2019 (in red) and Fall 2020 (in blue). Because clinicians are able to “check all that apply” for each student, the theoretical range for each concern is 0 to 100%. Actual prevalence rates range from a low of 0.2% for a pregnancy-related concern in the Fall 2019 to 66.8% for anxiety in the Fall 2020.
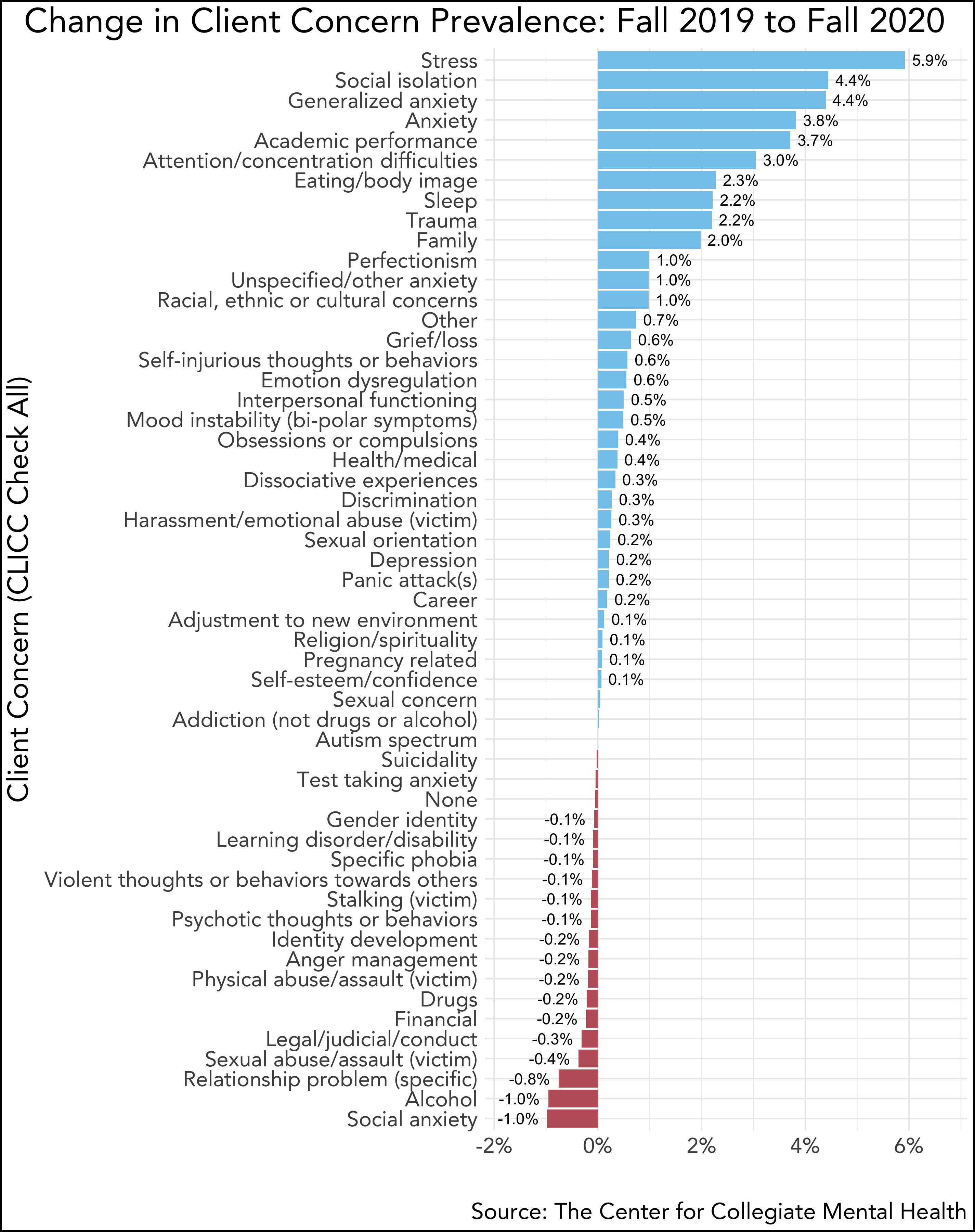
To provide a more clear illustration of how presenting concerns changed between Fall 2019 and Fall 2020, the chart below highlights the raw percentage change for each presenting concern between Fall 2019 and Fall 2020. Concerns at the top of the chart (in blue) increased in Fall 2020 whereas concerns at the bottom (in red) decreased in Fall 2020. Presenting concerns demonstrating the greatest increase during Fall 2020 included stress, social isolation, generalized anxiety, academic performance, attention/concentration difficulties, eating/body image, sleep, trauma, and family. Presenting concerns demonstrating the greatest decrease for Fall 2020 included: social anxiety, alcohol, and relationship problems.
Summary and Suggestions
In this blog, Part 2 of 5, CCMH examined how mental health (self-report and clinician evaluation) changed among treatment seeking students from the Fall 2019 to Fall 2020.
- Student self-reported distress increased slightly and temporarily in the areas of Eating Concerns and Family Distress, whereas Academic Distress demonstrated a more substantial and sustained increase. Other areas of distress (Depression, Generalized Anxiety, Social Anxiety, Alcohol Use, Hostility, General Distress, and Suicidal Ideation) remained relatively stable from Fall 2019 to Fall 2020.
- When specific symptoms of the Depression and Generalized Anxiety subscales were further explored, some symptoms increased (isolation, sleep difficulties, being easily frightened, racing thoughts, general fear, and tension), but these increases were offset by decreases in other symptoms, such as fear of having panic attacks in public and suicidal thoughts.
- The prevalence of clinician identified presenting problems increased in several areas, including stress, social isolation, generalized anxiety, academic performance, attention/concentration difficulties, eating/body image, sleep, trauma, and family. These trends were largely consistent with students’ self-report data.
While these trends confirm that student mental health has been impacted during COVID-19, they also reinforce that the nature of changes are nuanced. The data reviewed here suggest remarkable consistency between increases in student self-reported distress and concerns identified by clinicians, particularly with academics, family, eating concerns, sleep, attention/concentration difficulties, and trauma. The one domain that initially appears to be somewhat incongruent is Generalized Anxiety (stable self-reported distress but increased via clinician assessments). However, on closer examination, CCMH found that most symptoms of self-reported Generalized Anxiety did increase (sleep difficulties, easily frightened, racing thoughts, general fear, and tension), but these increases were offset by a significant decrease in concern about panic attacks in public. Given that public behavior has significantly declined during COVID-19, it is understandable why this specific symptom decreased whereas most other symptoms of Generalized Anxiety increased.
Comparing pre and post-COVID-19 onset time periods, this data makes clear that COVID-19 is negatively impacting many aspects of students' lives. These data indicate that colleges and universities should be preparing to specifically support the mental health needs of students during COVID-19, especially in the areas of academic distress, family, eating concerns, trauma, and anxiety, among others. In addition, some of the decreases in presenting concerns should serve as a red flag for institutions when planning for return to campus. For example, decreased anxiety (social, panic, etc.) may be positive in the short-term, but a year of isolation and reduced opportunities to experience and overcome anxiety symptoms may lead to greater levels of anxiety upon return to a social campus environment. Similarly, a year of distance from social/emotional/interpersonal interactions and access to drugs and alcohol may interact when students return to the campus environment and cause a spike in related concerns.
It should be particularly noted the clinical data reviewed by CCMH confirm that students are struggling with the remote academic environment, and this struggle seems to be compounded by living at home and simultaneously managing family dynamics and various forms of anxiety. While there are certainly benefits and silver-linings tied to the remote-learning experience, these benefits appear to be limited. Overall, it will be essential for colleges and universities to be attentive, resourced, and creative to address the ongoing and future challenges encountered by students due to the pandemic, including thoughtful preparations for programming, services, and support as they re-integrate students to an in-person student experience.
Please stay tuned for Part 3 of the CCMH COVID-19 Blog series where we will explore the impact of COVID-19 on the mental health of various identity groups.

